Helping Children Reach their Potential
You can search for courses, events, people, and anything else.
An immunologist by training, Dr Tara Roberts wasn’t planning to study cancer. In an effort to find out how genes affect cellular responses to DNA damage, she engineered mice to have only one working copy of a gene called SMG1, and was surprised to find a dramatic increase in the incidence of lung tumours and blood cancers. “It was one of those serendipitous discoveries,” says Roberts, who published her findings in 2013 in the Proceedings of the National Academy of Sciences of the United States of America. A year later, she landed a job at Western Sydney University with a dual appointment at the Ingham Institute for Applied Medical Research, where she created the Cancer and Inflammation research group that would apply immunological expertise to oncology.
Her team’s first order of business: determining how exactly SMG1 is implicated in tumour growth. As Roberts reported at major cancer meetings last year in Australia, Europe and the United States, her group showed that in cell lines, the loss of SMG1 resulted in elevated levels of a critical protein complex called mTOR, one with known links to aberrant signaling pathways involved in cancer proliferation.
Clinical collaboration
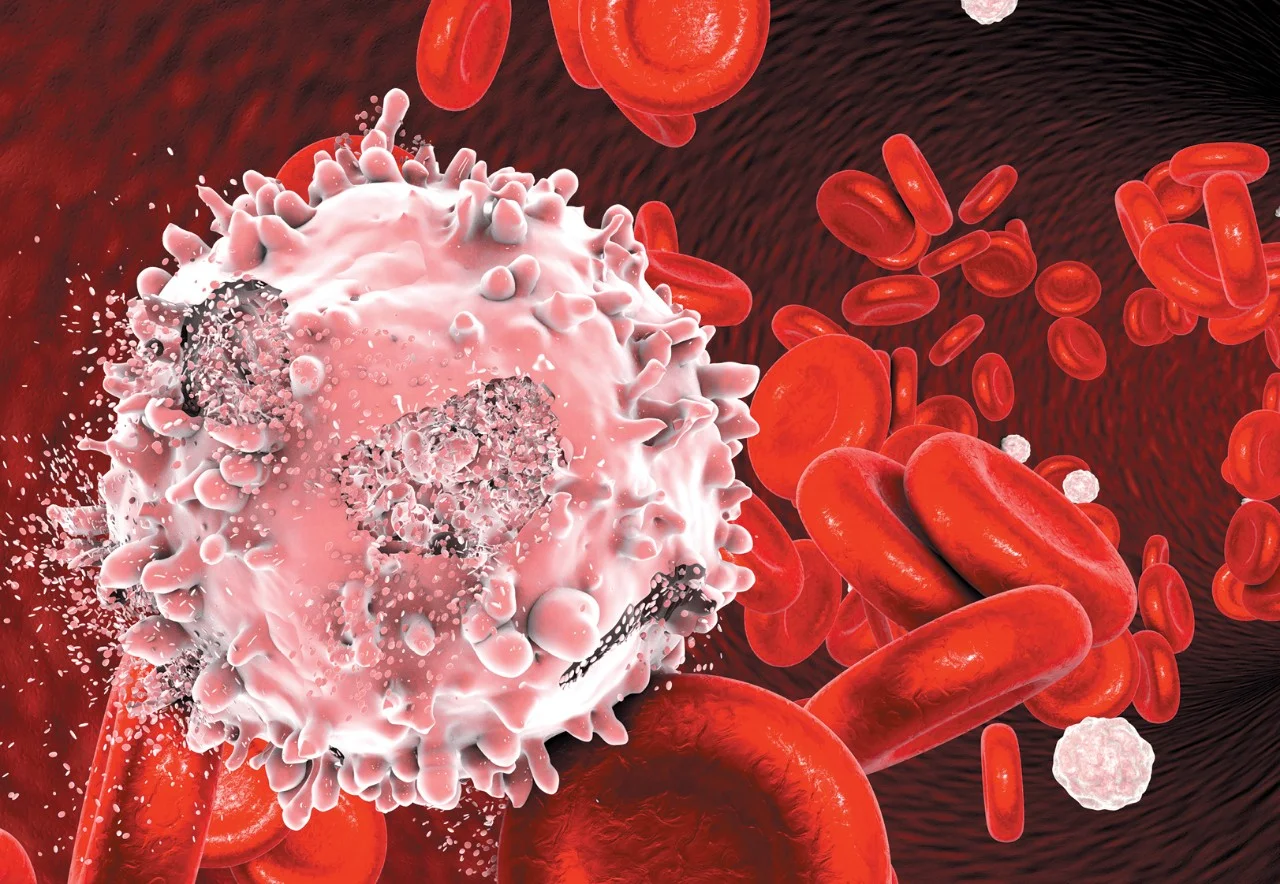
To examine the clinical relevance of SMG1 activity, Roberts and her PhD student, Patricia Rebeiro, collaborated with haematologists from Liverpool Hospital, and biobank managers from the Cancer Institute NSW’s Centre for Oncology Education and Research Translation (CONCERT) to collect blood samples from patients with chronic lymphocytic leukaemia, a slow-growing cancer that affects a type of white blood cell.
They found that around a third of these patients had no detectable levels of the protein encoded by the SMG1 gene in their bloodstream. What’s more, in these same patients, cancer cells showed signs of increased mTOR signaling. That suggested the loss of SMG1 could make cancers more susceptible to mTOR-blocking agents, a premise supported by preliminary lab tests on patient samples.
Roberts and her colleagues exposed cancer cells to an experimental mTOR-targeted drug called sapanisertib, now in mid-stage clinical trials. They discovered that, among cells lacking SMG1 activity, “there was more growth suppression and cancer cell death in response to mTOR inhibition,” Roberts says.
This finding could have significant impact, notes study co-author, and CONCERT programme manager, Nicole Caixeiro, who credits Roberts’ multi-disciplinary training and openness to collaboration for making the project possible. “Roberts is one of those basic scientists who appreciates the importance of research that is inclusive and calls upon all different health professionals,” Caixeiro says.
Need to know
- The enzyme encoded by SMG1 regulates inflammatory responses
- The loss of SMG1 could make cancers more susceptible to mTOR-targeted drugs now in clinical testing
- An interferon inducing pathway can affect whether cancer patients respond to immunotherapy drugs
Common Pathways
Before coming to Western, Roberts had also been studying the role of inflammation in ataxia telangiectasia, a neurodegenerative brain disorder caused by mutations in a gene called ATM. In rat models, she and her colleagues from the University of Queensland showed that the loss of ATM leads to the activation of an immune signaling molecule, called interferon, that underpins neuroinflammation in the brain.
Bringing her research full circle, this same interferon inducing pathway was shown to determine a cancer patient’s response to the latest life-saving immunotherapy drugs. Roberts is now examining how this may be exploited to determine the best treatment for individual cancer patients.
Meet the Academic | Dr Tara Roberts
Dr Tara Roberts is a Senior Lecturer in Oncology at the School of Medicine and Cancer Institute NSW Future Research Leader Fellow at the Ingham Institute for Applied Research. Dr Roberts completed her PhD at the Institute for Molecular Bioscience, University of Queensland.
In 2007, she was awarded an NHMRC Peter Doherty Fellowship and moved to the Queensland Institute of Medical Research. In 2014 she accepted a Cancer Institute New South Wales Future Research Leader Fellowship to start work at the Ingham Institute and Western Sydney University. This role involved the establishment of a new research group “Cancer and Inflammation”. This group utilises molecular and cellular biology techniques and analysis of animal models and patient samples to understand how certain mutations change the biology of cancer cells with the aim of exploiting these differences to improve patient treatment.
Related Articles
Credit
This project was funded by the Cancer Institute New South Wales.
© KATERYNA KON/SCIENCE PHOTO LIBRARY/ Getty Images; © puruan/ Getty Images
Future-Makers is published for Western Sydney University by Nature Research Custom Media, part of Springer Nature.