You can search for courses, events, people, and anything else.
Traditional Chinese Medicine and Western medical practice can be complementary approaches to healing. That’s the philosophy of Western Sydney University Associate Professor Carolyn Ee, a practicing GP and academic lead at NICM Health Research Institute’s joint initiative and partnership of Next Practice — Western Sydney Integrative Health (WSIH), Australia’s first university-based integrative healthcare centre.
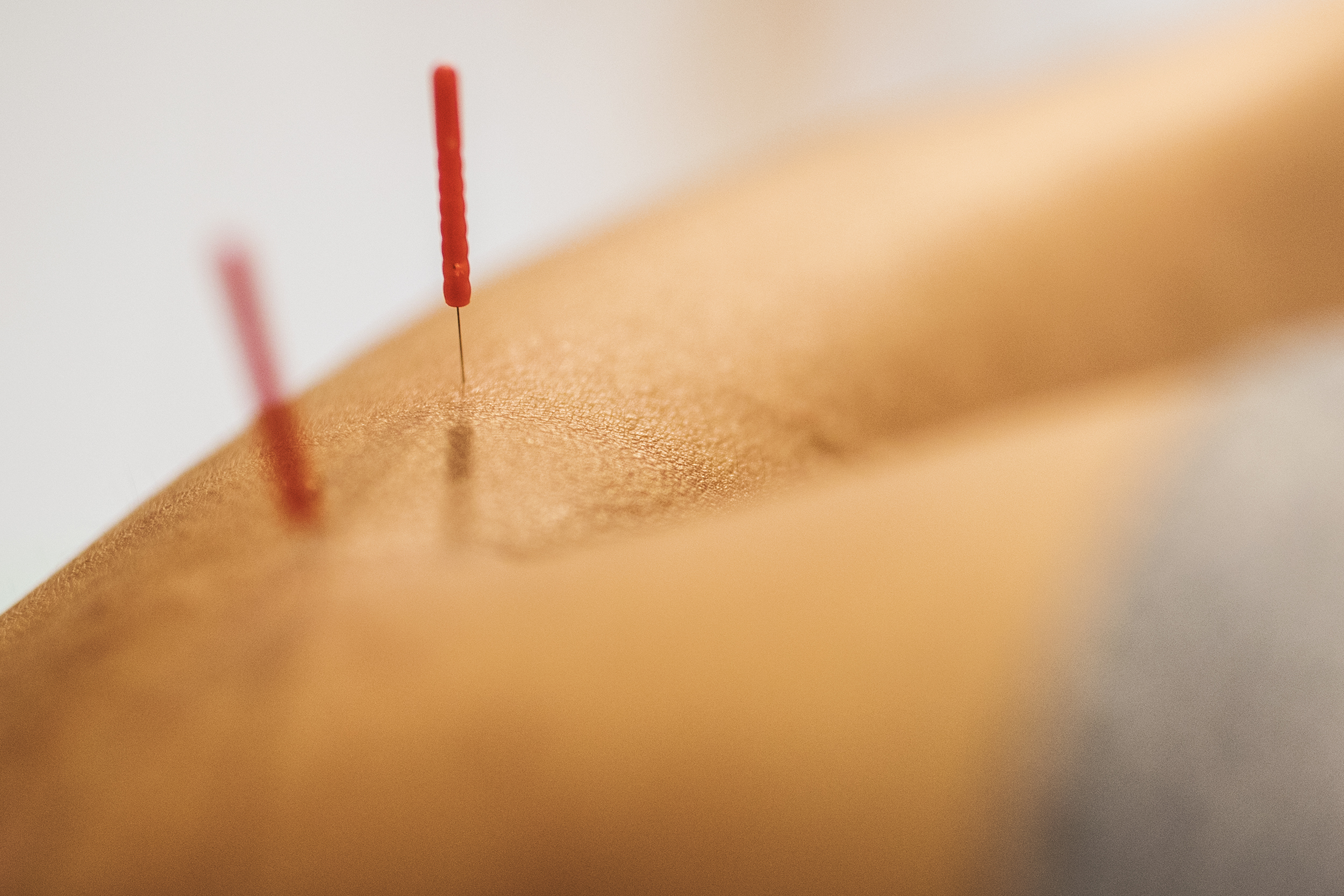
Launched in February 2022, the centre integrates general practice with complementary therapies, including yoga therapy, acupuncture and the use of dietary supplements. The integrative medical centre hopes to help alleviate symptoms of illness, and the side effects of prescribed drugs, experienced by people with chronic conditions or cancer. "Western medicine can save your life, but integrative medicine can make your life worth living," Ee says.
COMPLEMENTARY MEDICINE
Ee has a long history in healthcare. "I joined medical school straight out of high school, and then jumped directly into being a junior doctor," she says. For Ee, the long hours were not the biggest challenge. "It was the sense that I wasn’t always able to help people,” she says. “Often patients came in because they were having a severe side effect to a prescribed medication, and at times it felt like I was in sickness care rather than healthcare."
In her third year as a junior doctor, Ee — who has a Chinese background and a long-held interest in the culture’s traditional medicine — took time out to consider other healthcare approaches.
She spent the next three years gaining a degree in Chinese medicine at RMIT University, before completing her specialist training as a GP to become one of the first practising medical doctors in Australia to also carry traditional Chinese medicine qualifications. "Then I started looking at how I might combine the two," she says.
Each system has distinct strengths, believes Ee. "Western medicine is very good at resuscitating you when you’re very sick. If you’re about to have a heart attack, I’m not going to prescribe yoga, I’m going to get you into an ambulance," she says.
In combination with Western medicine, complementary medicine can assist with treatment of symptoms and side effects, and recovery. "If you have cancer you need the chemotherapy and radiotherapy, but you can certainly do other things to help reduce the side effects, so acupuncture can help with the pins and needles that you might get from chemotherapy, or yoga might help with the fatigue from radiotherapy."
While working as a clinician, Ee became interested in integrative medicine research after using acupuncture to help women who were experiencing menopausal hot flashes. "The acupuncture seemed to work, and I wanted to know why," she says.
Ee’s team conducted two clinical trials, comparing acupuncture with a type of placebo acupuncture that uses blunt false needles that retract before they puncture the skin. The studies showed that, in both groups, around 40% of treated women experienced a reduction in hot flashes. "So we concluded that acupuncture seemed to work, but it’s nothing to do with the actual needle going through the skin," Ee says.
"There may be a kind of beneficial effect that comes from the therapeutic interaction of attending the clinic and talking about the symptoms," she adds. In a secondary analysis of her trial data, Ee also showed that the patient’s odds of getting better had no correlation with their expectations of recovery before the treatment began, proving that women didn’t just get better because they expected to get better.
INTEGRATIVE HEALTHCARE
In 2016, Ee joined Western Sydney University’s NICM Health Research Institute, which specialises in research on traditional, complementary and integrative therapies, to continue her work. Her recent work has investigated the benefits of integrating complementary medicine with typical treatments for women’s health issues, for cancer survivorship, and for patients who have metabolic conditions such as diabetes and obesity. Cancer is currently her main focus, alongside heading up Next Practice WSIH.
"The idea for the integrative health centre emerged because NICM Health Research Institute wanted to explore how we could translate our research into practice," Ee says. University-based, evidence-led integrative health centres combining general and complementary practice are already common at universities, research clinics and cancer centres in the United States. So Ee led a series of studies examining the potential value of establishing the first such centre in Australia.
"Our first consumer survey highlighted how much the centre was needed," Ee says, pointing to the trust and credibility brought by a university-based initiative. In subsequent studies, the team established that local GPs and medical specialists would strongly support an integrative health centre that was evidence-based and focused on patient safety.
The centre has been embraced by local healthcare practitioners. "It’s a great resource for our patients," says Elisabeth Elder, a breast surgeon at the Westmead Breast Cancer Institute and clinical professor at the University of Sydney. "Carolyn and her team are also wonderful collaborators on a number of research projects with the aim to improve long-term well-being for people with cancer from different backgrounds," she says.
Strengthening the evidence base of integrative healthcare through research remains the focus of Ee’s work. The team is developing summaries to guide centre practitioners on the latest research findings about different therapies for specific patient needs. The emphasis on evidence also extends to the outcomes of the centre’s own patients, Ee adds. "We’re starting to collect patient outcome data including measures of quality of life, pain, depression, and patient satisfaction, so that we can see the real-world impact our integrative medical centre is having."
Meet the Academic | Associate Professor Carolyn Ee
Dr Carolyn Ee is an academic GP and was one of the first practicing medical doctors in Australia to gain dual qualifications in Chinese Medicine.
Her research vision is to have a measurable impact on the lives of people with chronic illness. To do this she leads a research team and program that creates, synthesises, and translates scientific evidence on the integration of non-drug therapies and Eastern medicine with Western medicine delivered in primary care. She has published more than 60 peer-reviewed journal articles.
Carolyn’s research focuses on metabolic conditions, women’s health, and cancer survivorship, and on integrative medicine health services and education more broadly. Her expertise spans randomised controlled trials, systematic reviews, qualitative research and guideline development and translation, and is built on a foundation of strong consumer and stakeholder involvement and engagement and translation into practice. Underpinning her research expertise is more than 20 years' experience as a medical doctor. She practises clinically as an Integrative Oncology and Supportive Care Specialist GP at a comprehensive cancer centre.
Carolyn’s leadership and prominence in the field are reflected in her appointments at international, national, and local levels. She is a well-known advocate for work-life balance and health and wellbeing for all. Her work has featured across key media outlets including The Age, New York Times, Reuters Health, ABC National, Prevention, The Conversation, NewsGP, SBS, and Today Tonight.
Credit
Future-Makers is published for Western Sydney University by Nature Research Custom Media, part of Springer Nature.