You can search for courses, events, people, and anything else.
By combining artificial intelligence with state-of-the-art radiation therapy for cancer, Western Sydney University researchers hope to be able to image the internal structures of tumours, which will enable clinicians to tailor cancer treatment.
The conventional way to treat tumours is to excise them surgically, but this generally requires a major operation, and some tumours are surgically inaccessible.
By replacing the scalpel blade with focused beams of X-rays, electrons or other subatomic particles, radiation therapy can treat tumours without cutting patients open. However, breathing and other bodily movements can cause tumours to move during treatment, and so surgeons must target a considerably larger region than the tumour. This can result in collateral damage to surrounding healthy tissue.
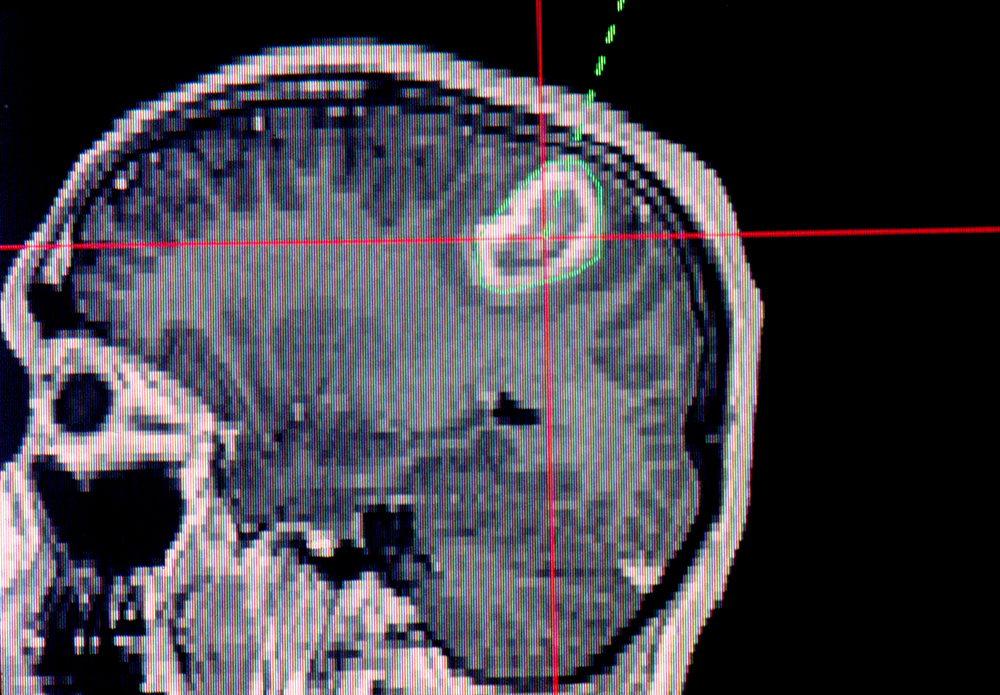
An exciting new treatment that promises to overcome this problem is MRI–LINAC. It integrates two key technologies that have been used separately for treating cancer into a single system. A linear accelerator (LINAC) delivers high-dose radiation, while magnetic resonance imaging (MRI) provides real-time imaging of the tumour. This allows clinicians to pinpoint tumours during treatment, drastically reducing the damage to nearby, healthy tissue.
Bringing these two technologies together was quite a feat of engineering since MRI requires very high magnetic fields, which can cause the radiation beam to veer off course. “They’re challenging technologies to combine in one machine, and so MRI–LINAC is a very recent development,” notes Professor Bill Price, from Western’s School of Science. As a result, there are only a handful of such machines in the world today.
Having devoted his professional life to researching MRI, Price is now working on the MRI side of MRI–LINAC. While MRI is a mature technology, he is convinced that it has a lot more to offer. “It’s come such an enormous way in the last three decades, but it still has so much untapped potential,” he says.
In particular, MRI can do more than just locate the positions of tumours — it can also reveal their internal structures. As part of a project funded by the Cancer Council NSW, Price and his team at Western are now exploring how to exploit this ability of MRI to precisely treat tumours using MRI–LINAC.
“For example, if part of the tumour is more resistant to radiation than the rest, then you can increase the dosage in that area,” explains Price. “If you can do that, you’re much more likely to have successful treatment and hopefully lower rates of recurrence.”
Price’s team is obtaining images on tissue samples that contain pancreatic, oesophageal, liver, and rectal tumours in the lab using ultrahigh-resolution MRI systems that use extremely high magnetic fields to image samples that are up to 3 cm in size. “Our lab MRIs have very high magnetic fields, and so they can give resolutions that greatly surpass what you can get on a clinical machine,” explains Dr Timothy Stait-Gardner, the National Imaging Facility Fellow in Western’s School of Science.
They then plan to use AI to apply the results to the lower resolution images obtained using (clinical) MRI systems in MRI–LINAC machines, which are designed to scan the whole body.
By comparing images taken on the same sample on a very-high-field MRI machine and a clinical MRI machine, the team intends to use AI to create algorithms that can greatly improve images taken on clinical MRI systems.
Price is excited about the project’s potential. “Feeding our results into MRI–LINAC promises to be fantastic. Instead of: ‘Oh, there’s a tumour, blast away,’ suddenly you can devise a treatment much more carefully,” says Price. “There should be better treatment, fewer side effects, less cancer recurrence and less damage to tissue that didn’t need to be irradiated.”
The ability to see inside tumours makes treatment tailored to individual patients much easier and quicker. “I hope that in the future we won’t need so many physical biopsies because treatment decisions could be made much faster and with less trouble for the patient using MRI,” says Price. “We could find out the extent of a tumour, what type it is, how heterogeneous it is, and if there are changes in pH or oxygenation, because all of these things affect treatment protocol.”
Meet the Academic | Professor Bill Price
Meet the Academic | Dr Timothy Stait-Gardner
Credit
Future-Makers is published for Western Sydney University by Nature Research Custom Media, part of Springer Nature.
This research was funded by the Cancer Council NSW Project Grant RG 22-02.
© Kateryna Kon/Science Photo Library
© Philippe Plailly/Science Photo Library
© drazenzigic/Freepik