Our Research
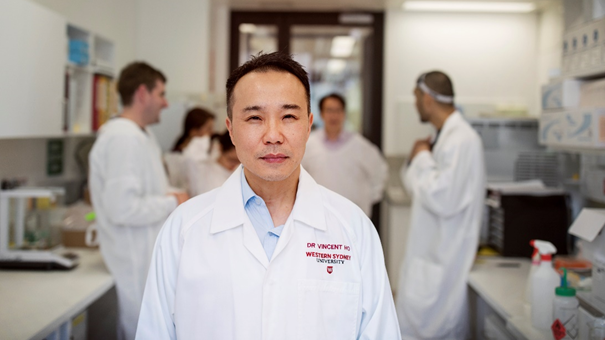
Dr Vincent Ho and Dr Jerry Zhou run the Translational Gastroenterology Laboratory at the School of Medicine, Western Sydney University. We are passionate about our research program because it holds the promise of improving symptoms, improving the quality of life and returning to patients with gastrointestinal disorders the meaningful lives they deserve. Our focus is on bench-side to bed-side research using the latest innovations and technology in the scientific field.
Clinical Trials
Clinical trials are an essential component of our translational research. They are research studies performed in people that are aimed at evaluating new methods of treatment, disease management, or diagnosis. Our laboratory is spearheading a number of trials involving the latest innovations in medical devices and clinical intervention. Some of our internally developed trials includes:
- Internet-of-things device for home-based anorectal biofeedback therapy
- Fecal transplant for individuals with irritable bowel syndrome and other gastrointestinal disorders
- Nano-endoscopy for office-based screening of reflux-associated disorders and oesophageal cancer
We also work with a number of external partners, leading clinical and pivotal trials for Nestle Health Science and Atmo Biosciences.

Gut Microbiome in Health and Disease
Bacteria and microrganisms play a pivotal role in gastrointestinal health. Microbiota homeostasis is an indicator of health while changes in microbiome profiles can predict or identify underlying diseases. We work with a range of partners including, local advocacy group (Oesophageal Cancer Awareness Group Inc.), dieticians (Designer Diets), and South West Sydney Local Health District. Our areas of research includes:
- Investigate the oesophageal microbiota changes associated with reflux diseases and its potential to develop an non-invasive screening tool of oesophageal cancer.
- Effects of prebiotic intervention of long-term gut microbiome modulation.
- Application of faecal transplantation in the treatment of irritable bowel syndrome.
Pace-makers of the gut
A PhD scholarship is currently available for this project. Find out how to apply.
A specialised population of cells found in the gastrointestinal tract, called interstitial cells of Cajal (ICC), are responsible for gastric pace-making and slow wave movement. Loss or absence of ICC have been linked with motility disorders, such as gastroparesis, slow-transit constipation, and irritable bowel syndrome. The isolation and analysis of these cells will provide a better understanding how the human gut works. We work with regenerative medicine expert A/Prof. Michael O'Connor and his team to molecularly profile live ICC derived from human gut tissue. This information will be used to establish ex-vivo cultures to lay the foundations of generating artificially-derived ICC and its application in regenerative therapy.

Would you like to be involved in our research?
Medical Device Development
We work with a multi-disciplinary team of bioengineers, programmers, and clinicians to develop innovative technologies to improve gastrointestinal health. We work closely with industry partners and collaborators including IDE Group, Atmo Biosciences, and Cicada Innovation. Current projects in development includes:
- New Internet-of-Medical-Things system for home-based anorectal biofeedback therapy.
- Portable endoscopy system for the rapid screening of reflux related diseases.
- Utilise machine learning to predict oesophageal diseases based on symptom behaviour in order to assign priority for downstream endoscopic investigation.

Improving clinical diagnosis of motility disorders
High-resolution manometry is a gastrointestinal motility diagnostic system that measures intraluminal pressure activity in the gastrointestinal tract. Our motility clinic at the Camden Hospital have access to the latest high-resolution oesophageal and anorectal manometry systems.
Oesophageal manometry is used to assess oesophageal motor function, by providing complete physiological mapping of the esophageal motor function, from pharynx to stomach. This advanced diagnostic technology allows us to evaluate causes of gastric reflux, difficulty swallowing, functional chest pain and pre-operative evaluation. Anorectal manometry is used to assess pressure activity of the rectum and anal sphincter. This advanced diagnostic technology allows us to evaluate patients with conditions such as impaired defecation, chronic constipation, rectal prolapse or Hirschprung's Disease.
Although powerful, these pioneering techniques are still in their infancy. Therefore, our clinical research team focuses on improving diagnostic yield and determine how to best utilize these technologies in our patients.


 GP Home
GP Home
